A 62 yearold gentleman presented to us with complaints of upper abdominal pain with radiation to back since 2 months. He also complained of weight loss, however this was not significant.
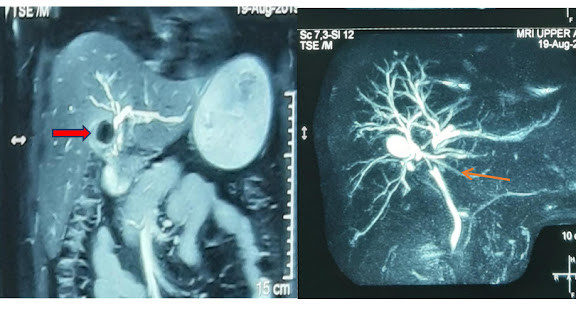
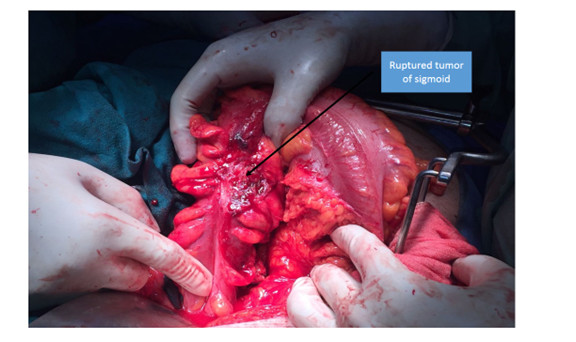
Ultrasound and contrast enhanced CT scan of the abdomen (figure 1) was suggestive of a cystic lesion in body and tail of pancreas. To further characterize the lesion a MRI with MRCP of the abdomen was done. This was suggestive of a mixed-micro & macro-cystic lesion in tail of pancreas. A communication between the lesion and pancreatic duct was demonstrated (figure 2). These features pointed to a branch duct intraductal papillary mucinous neoplasm (BD-IPMN). An endoscopic ultrasound (figure 3) was suggestive of a mixed micro- and macrocystic lesion of pancreas and myxoid material was aspirated. The cyst fluid amylase and CEA was 154 U/L and 0.12 ng/ml respectively and were normal, indicating a non-mucinous cyst.
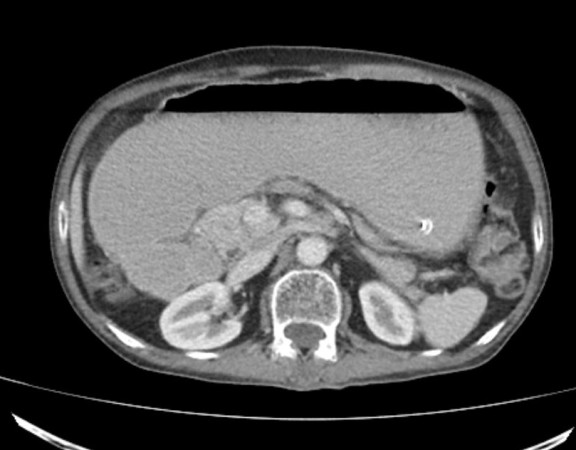
In view of these findings which raised a suspicion for IPMN on imaging, the patient was counselled regarding surgery. After thorough preoperative preparation and evaluation, the patient underwent distal pancreaticosplenectomy (resection of part of body, tail of pancreas along with spleen) (figure 4). Postoperative recovery was uneventful. Histopathology was however suggestive of serous cystic neoplasm (SCN).
A rise in the incidence of cystic lesions of pancreas has been noticed. This has paralleled an increase in the use of cross-sectional imaging. These cystic lesions present either as incidental findings on imaging studies performed for evaluation of an unrelated condition or with symptoms. The main cystic neoplasms of pancreas include
- Serous cystic neoplasm (SCN)
- Mucinous cystic neoplasm (MCN)
- Intraductal papillary mucinous neoplasm (IPMN)
- Solid pseudopapillary epithelial neoplasm (SPEN)
The cystic neoplasms like SCN areinnocuous in nature, while MCN and IPMN have a definite malignant potential. These cystic lesions require a careful multidisciplinary evaluationat centers with experience.
The evaluation is in the form of cross-sectional imaging preferably MRI and MRCP and endoscopic ultrasound. These investigations help in clarifying the nature of the cystic lesion. An EUS also helps in guiding needle aspirationsof cyst fluid and from suspicious area, the results of which can help in deciding the management plan. The aim of this evaluation is to differentiate benign cystic lesions from those with a malignant potential.
In general, surgery for these lesions is advised in case these cysts give rise to symptoms, or the imaging features are suggestive or confirmatory of lesions with a malignant potential(MCN, IPMN) or in case imaging features suggest or confirm a malignancy.Surgery for these lesionsrequires a pancreatic resection either in the form of whipple’s procedure, distal pancreatectomy with or without splenectomy or sometimes a total pancreatectomy. The pancreatic resections are usually associated with its own set of complications. Therefore, a thorough preoperative preparation and evaluation for fitness for surgery is a must. It has also been clearly shown that results of these surgeries are significantly better at centers with expertise and experience.
In our patient, although the final pathology revealed SCN (lesion with negligible malignant potential), surgery was still advisable because of presence of symptoms and imaging features suggestive of a cyst with malignant potential.
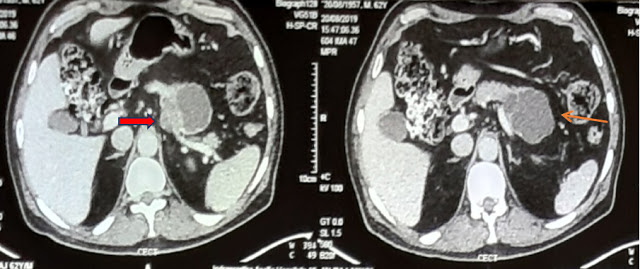
Figure 1 Contrast enhanced CT abdomen suggestive of a cystic lesion of pancreas with mixed microcystic (bold arrow) and macrocystic (thin arrow) component.
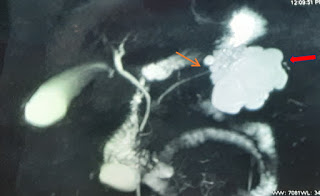
Figure 2 MRCP suggestive of a lobulated macrocystic lesion of pancreas (bold red arrow) with a demonstrable communication with main pancreatic duct (thin arrow).

Figure 3 Endoscopic ultrasound showing a mixed macrocystic (marked by red star) and microcystic lesion (marked by yellow star)
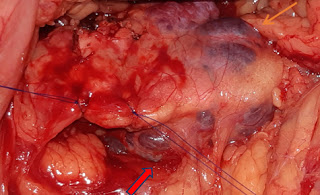
Figure 4 Intraoperative photograph showing stay sutures on either side of the site planned for transection. The lesion involving the body of pancreas can be appreciated (posterior border marked with bold arrow and anterior with thin arrow).
Dr Aishwarya Jain
DrRigvedGupta
Dr Varun Madan
Dr Abhishek Mitra
Dr Deepak Govil
Department of Surgical Gastroenterology and Gastrointestinal Oncology
Indraprastha Apollo Hospital
Sarita Vihar
New Delhi