Mirrizi’sSyndrome- Stone in Gallbladder Remnant Resulting in High Biliary Stricture- a challenging scenario
A 34yearold gentleman, a known case of diabetes and hypertension, underwent surgery for symptomatic gallstones in December 2018 at an outside hospital. The surgery was started laparoscopically but converted to open procedure. As per the surgeon’s notes the reason for conversion was a technically difficult cholecystectomy. The histopathology of the removed gallbladder was suggestive of chronic cholecystitis. Postoperatively a CT guided drainage of intra-abdominal collection was done. Thereafter, he recovered from the procedure and was asymptomatic.
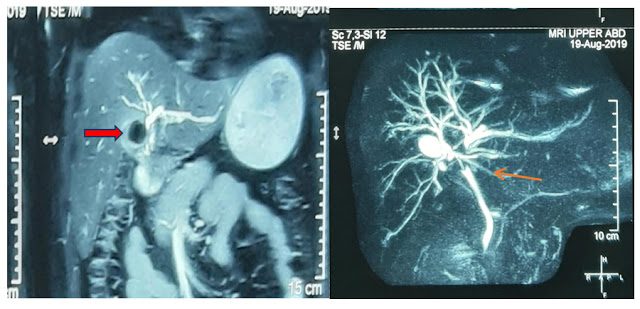
He visited our department with an ultrasound report showing a stone in gallbladder remnant with dilated biliary system. The liver function tests were suggestive of biliary obstruction (raised ALP and GGT). MRCP was suggestive of a gallbladder remnant along with large calculus (2 cm) in GB bed with compression at biliary confluence along with dilated intrahepatic biliary radical dilatation (Figure 1). This picture was suggestive of a Mirrizi’s syndrome.
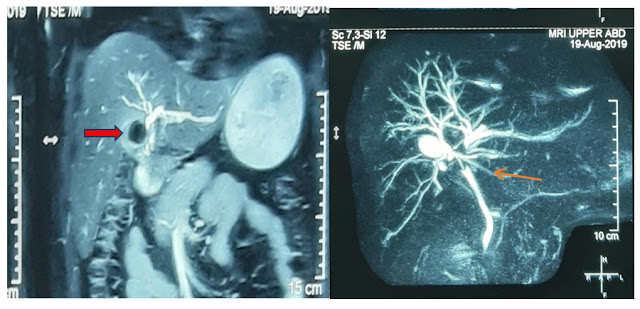
Figure 1 MRCP suggestive of gallbladder remnant with stone (red arrow) leading to compression/stricture (orange arrow) at biliary confluence.
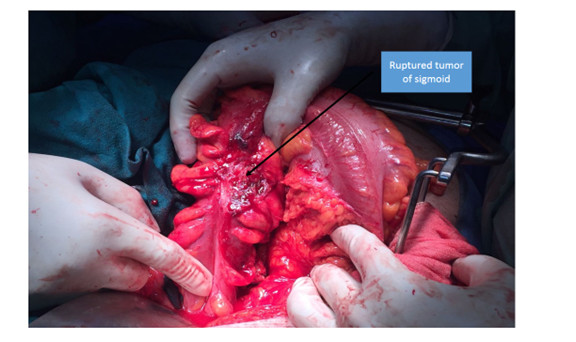
He was prepared for open procedure- cholecystectomy and hepaticojejunostomy after obtaining preoperative fitness and informed and written consent. Introperatively there were dense adhesions of colon and omentumto the porta hepatis. The liver was also densely adherent to parietal wall. After careful dissection, the thick-walledremnantgallbladder was identified. This was densely adherent to porta structures. The gallbladder was opened and the large impacted stone was removed. A fistula between the gallbladder and common hepatic duct was suspected after removal of stone. To confirm the presence of fistula and to delineate the anatomy further, a cholangiogram was obtained through a tube placed in gallbladder remnant.
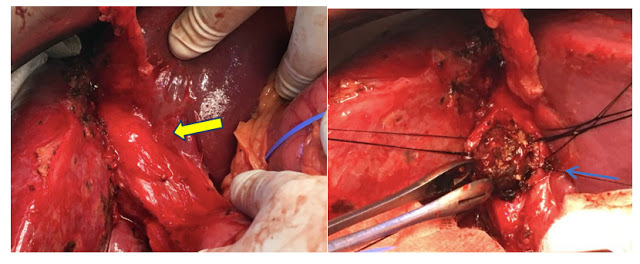
Figure 2 Gallbladder remnant adherent to porta hepatis (yellow arrow). Gallstone removed after opening the gallbladder remnant (blue arrow).
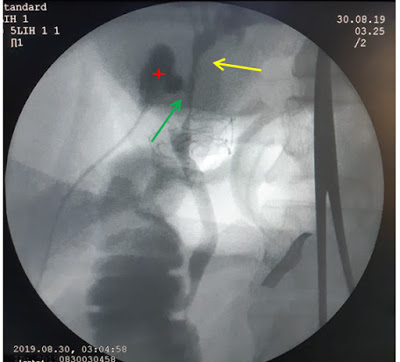
Figure 3 Intraoperative cholangiogram through tube placed in the gallbladder remnant (red cross) showing fistulous communication (green arrow) with the common hepatic duct and stricture starting just below the biliary confluence (yellow arrow).
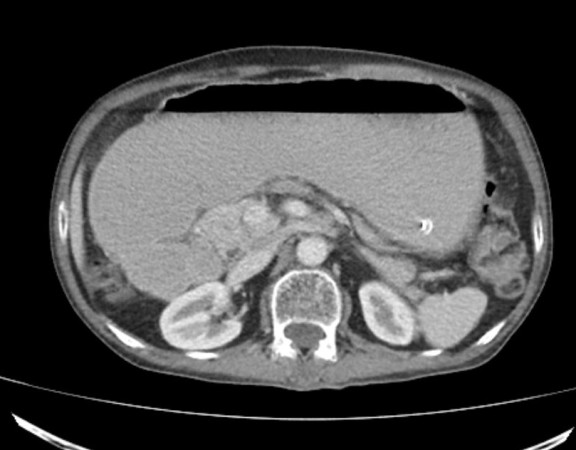
In view of these findings, the gallbladder remnant was dissected carefully from the porta structures and resected. The biliary confluence was identified and opened widely for anastomosis. A Roux-en-Y hepatico-jejunostomy was performed. A T tube was placed across the anastomosis. Postoperative period was uneventful. He was discharged on postoperative day 9. Histopathology of the removed gallbladder was suggestive of acute on chronic cholecystitis. T tube cholangiogram done at 3 weeks was suggestive of a patent anastomosis with no contrast extravasation and T tube was removed. He has been asked to follow up after 6 months.
Mirrizi’s syndrome results from compression of the bile duct as a result of stone impacted in the gallbladder neck or cystic duct. These patients usually present with jaundice, pain and/or fever (features of cholangitis). The presentation can mimic that of a malignancy. A thorough radiological evaluation is required in these cases and this diagnosis must always be considered in all patients with an impacted gallbladder stone with biliary obstruction. The surgery itself is challenging because of altered anatomy and an increased risk of biliary injury. Although, the procedure can be attempted laparoscopically, the chances of conversion to an open approach is higher than a routine gallbladder surgery. The surgical procedures that one needs to perform for this challenging problem depends on the extent of involvement of the bile duct. These include cholecystectomy alone, bile duct repair and hepaticojejunostomy. Hence, these challenging procedures should preferably be performed at high volume centers with experience.
In our case, the patient presented to us with an asymptomatic rise in liver enzymes. However, imaging was suggestive of a biliary obstruction. We chose an open approach, as we anticipated a difficult procedure. The use of intraoperative cholangiogram helped us in further delineation of the anatomy. T tube was placed across the anastomosis as a security, given the extent of biliary inflammation.
Mirrizi’s syndrome is a challenging presentation of gallstone disease and requires a high index of suspicion. The management is mainly surgical. The procedure requires careful delineation of the anatomy and extent of the biliary involvement. These surgeries should preferably be performed at high volume centers with expertise.
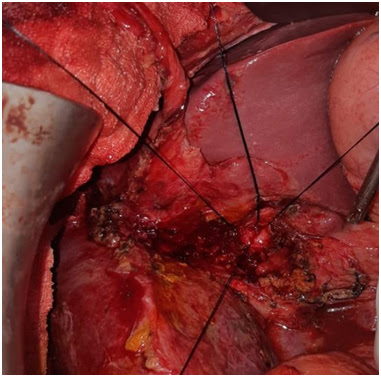
Figure 4 Intraoperative photograph showing silk stay sutures on the anterior and posterior aspects of the biliary confluence
Dr Aishwarya Jain
DrRigvedGupta
Dr Varun Madan
Dr Abhishek Mitra
Dr Deepak Govil
Department of Surgical Gastroenterology and Gastrointestinal Oncology
Indraprastha Apollo Hospital
Sarita Vihar
New Delhi